writing
TOPSY GOES TO NORWAY
On a misty morning in November 1957 a small furniture van left Bristol, heading north. In the passenger seat was William ‘Bunny’ Warren, a former RAF radar technician who had had dismantled, packed and secured the half-ton of kit the van carried. Known affectionately as ‘Topsy’, in the pre-digital 1950s that ‘kit’ was the most advanced brain investigation tool on the planet.
They followed a sedan, maybe a Humber, or Rover, in any event the sort of solid respectable car a senior hospital consultant would drive. Duggie Phillips was a brain surgeon, still a fairly rare bird in the newish National Health Service. Next to him was Harry Crow, an ironmonger’s son from Aberdeen. After a war spent navigating Mosquito bombers over occupied Europe Harry had returned to his hometown to recover, play rugby, and train as a doctor. Once qualified, he travelled south again, to London then Bristol, pursuing an interest in the brain.
In back were the boffins: Grey Walter and Ray Cooper. Grey was public school and Cambridge, a physiologist whose hobbies included cybernetics, robotics and writing science fiction; the only member of the group with a YouTube clip to his name. It concerns a small self-steering robotic tortoise that featured in the 1951 Festival of Britain. Ray Cooper was grammar school and Manchester; a draper’s son from Lancashire who never lost his accent, Ray graduated in physics at 19 and came to brain research via RAF radar and a PhD in astronomical optics. His snapshot and brief account will be the only enduring record of their trip.

Oslo, November 1957. Left to right: Harry Crow, Grey Walter, Dougie Phillips, Bunny Warren (courtesy of Ray Cooper, who took the photograph)
Their destination was RAF Fairford, in the heart of rural Gloucestershire, and as they near the security barrier my mind’s eye shifts into ‘50s film noir. The car and van emerge from the mist, to be halted by an armed US soldier. ‘RAF’ Fairford had been leased to the US Air Force since 1950. They extended the runway making it the longest in Europe and able to take the largest Cold War bombers. Their silver bulk looms as the convoy clears security and makes its way to more modest transport: a US Air Force C47 Skytrain, the World War II Dakota. It would not be a comfortable ride. Cruising at only 160 mph their flight to Norway would take five hours, and a blanket of fog over Oslo make for an anxious landing.
They came from the Burden Neurological Institute*, a private research establishment on the outskirts of Bristol. Why was the US Air Force acting as taxi service for five UK brain scientists; how did a psychiatric hospital in Norway, then one of Europe’s poorer countries, come to host one of the world’s most advanced neuroscience laboratories? This essay addresses those questions.
+
On 4th October 1957, a month before the Oslo trip, the Soviet R7 rocket successfully put an object into orbit around the earth. ‘Sputnik’ weighed as much as a small fridge and emitted a simple electronic ‘beep’ as it passed over the United States of America, four times a day. The following month the attempted to put their satellite into orbit. The rocket failed to clear the launch pad. In response Edward Teller, the father of the American atom bomb, went on national television and announced that the USA had lost a battle more important than Pearl Harbour: If the Soviets could put an object that size into orbit they could project a warhead between continents.
Earlier that year President Eisenhower had commissioned a US Senator to draw up a report on “Defence and Survival in the Nuclear Age’. The ‘Gaither Report’, delivered on 7th November 1957, was leaked to the Washington Post. It recommended a major investment in missiles and shelters. “Only through an all out effort…can the US hope to close the current missile gap to counter the world wide Communist offensive in many fields and many lands”. Missiles and shelters were only part of the response. Cold War paranoia, fuelled by Sputnik and the report, led to a funding windfall that spread to many fields, including, remarkably, neuroscience. In fact the military had been looking over the shoulders of brain scientists since the late 1940s, and in that field also the Soviets seemed ahead of the game. Ivan Pavlov was the leading experimental psychologist of the first half the 20th century. Mid century the best-known neuropsychologist was another Russian, A.R.Luria. He learned his trade studying the brain-injured veterans, who were plentiful in the Soviet Union.
Understanding and controlling the brain became a major concern of the military and intelligence communities in the West during the Korean War. The sight of American soldiers denouncing their government and way of life only days after capture was truly shocking and could only be explained, so went the thinking, by some form of mind control. “Brainwashing” was the term coined by a C.I.A. operative, and picked up by the popular press. Thereafter, the military, and particularly the C.I.A. funded experiments on a wide range of subjects thought relevant to mind-control. Some, such as the work of Jose Delgado at Yale, was funded openly, and the results published in military journals. Delgado wanted to control behaviour by electrical stimulation of areas deep inside the brain, through inserted electrodes. It was Delgado who, famously, stopped, or at least diverted, a charging bull via electrodes inserted deep in the creature’s brain and activated by a radio signal. In Delgado’s vision of the ‘brave new world’ violent criminals, paedophiles and other ‘undesirables’ would be similarly ‘psychocivilised’.
The C.I.A. favoured covert funding. Between 1955 and 1961 over 800 studies were carried out in more than 300 institutions as part of their MKULTRA programme. They included the use hypnotism and techniques used by magicians, but it was their study of LSD in interrogation that brought the programme to public attention. An employee jumped out of a high hotel window whilst ‘tripping’ in work time and his family looked for an explanation. When a Senate Committee sought information on this work in the mid 1970s they found no operational records. Richard Helms, the head of the C.I.A. from 1966 to 73, had ordered them destroyed before he left office. It was later found that he forgot to bin the accounts and his successor, Richard Colby was more open in his approach.
Another area of interest to the military was ‘conditioning’, the linking of stimulus and response much studied by Pavlov. In Richard Condon’s 1959 novel ‘The Manchurian Candidate’ a ‘brainwashed’ Korean War veteran is conditioned to assassinate the president in response to a particular stimulus (a playing card) as part of a Communist plot to take over the US. The novel was made into a successful film starring Frank Sinatra, and released in October 1962 during the Cuban missile crisis. A year later, when the president really was assassinated, Sinatra insisted the film be withdrawn from distribution. It was re-made in 2004, updated to Desert Storm, ‘Manchurian’ now referring to a multinational company with similar ambitions, and devices implanted in the brain as the agent of control.
In an unpublished memoir, written in the 1970s, Grey Walter describes how the Burden Neurological Institute became involved with the military:
My experience with supervision (private teaching) in Cambridge had established several ‘professional’ friendships with young men…One of my pupils had been a young American reading Medicine; we had swapped yarns about the states as well as discussing his essays. One morning I was sitting, wondering how the Institute would make ends meet, when he put his head around the door and said “Hi Grey!”. He was in USAF uniform, a colonel, and told me he was head of the U.S. Air Force Research Centre in Brussels. Did I want any money?.
Ray Cooper elaborated in his later book on the Burden:
Experiments in conditioning had been done at the Institute since the beginning and much time had been spent in the middle and late 1950s (with the aid of the Air Research and Development Command of the IS Air Force) looking with Topsy at the events in the brain that occur when a person uses one stimulus (S1) to prepare for action on receipt of a second stimulus (S2) a short time later.
Although Walter attributes his good fortune, in attracting US military funding, to a long-standing personal relationship, there was another reason why he would have been attractive to the military. After gaining a first in physiology at Cambridge he stayed on, carrying out research he hoped would lead to a fellowship. But after two years his project ran into problems and so he was offered a short-term research attachment. I.R. Rozental, one of Pavlov’s associates in Leningrad, was visiting Cambridge carrying out a project supervised by his master, on the effect of drugs on conditioning in dogs. For several months Walter became his assistant and in a letter to Pavlov Rozental expressed his hopes for his new pupil:
Barcroft found a very capable and knowledgeable young man named Walter for ‘processing’. It looks like he has an interest in conditioned reflexes… if he will commit and throw himself into our cause then the future of the conditioned reflex is guaranteed. I am trying to enthuse him.
(Letter dated March 1935, From the Pavlov Archive Leningrad, courtesy of Phil Husband)
At a time when the US military sought to understand all aspects of conditioning Walter’s experience was unusual and of interest as they strove to catch up in a field that seemed key to communist brainwashing techniques. In any event it seems likely Walter made the most of the experience. The flight to Oslo was part the resulting funding windfall. Incidentally, there is no record of the military projects undertaken in that decade in the Burden archive held by the Science Museum.
The Bristol group travelled at the invitation of Dr Carl Sem-Jacobsen, a Norwegian physician and brain scientist formerly based in the US. He had worked in a programme at the Mayo clinic that involved inserting electrodes deep into the brain and leaving them in place for weeks and months. Such electrodes could be used to electrically stimulate targeted brain areas, or at higher voltage, coagulate brain tissue. Electrophysiological recordings could also be taken. Patients with epilepsy and psychiatric disorders were the main groups investigated and treated and the last paper Sem-Jacobsen published before leaving the States was an account of ‘depth electrode’ studies of 93 psychotic patients. Most, if not all of those ‘subjects’ would have been long-term residents of psychiatric hospitals, many incapable of giving informed consent. By current standards such work seems jaw-droppingly unethical, but in the 1950s few would bat an eyelid. The paper was presented in the author’s absence at a Scandinavian psychiatric congress and followed by comments from Ørnulv Ødegår, one of Norway’s most senior psychiatrists and the long-serving superintendent of Gaustad Hospital, Oslo. After the paper had been delivered he comments that the work ‘may mark an entirely new era in psychosurgery’ and goes on to express the hope that Sem-Jacobsen would ‘continue these experiments on his return to Norway’. The following year he provided facilities in his hospital, and on-going US funding was promised. The low level of medical litigation in Norway, compared to the US, made the country especially appealing. Sem-Jacobsen had extended the invitation to Walter and his team when they met at a conference. The group included Walter, a physiologist, a physicist, electronics technician, neuropsychiatrist and neurosurgeon. Their aim was to learn the technique of electrode insertion, deep brain recording and coagulation and begin their own series back in Bristol.
+
In the middle years of the last century damaging the front of the brain as a way of treating mental illness, ‘leucotomy’, became popular in many countries, but Norway’s experience of the operation deserves particular comment. Before off shore oil was discovered and extracted in the 1960s Norway was one of Europe’s poorer countries, particularly after the German occupation in World War 2. Brain surgery of any type was expensive and in short supply. When the low cost ‘transorbital approach’ was developed by Walter Freeman in the US Ødegår at Gaustad became one of its most enthusiastic proponents. In consequence, by 1957 several hundred patients had undergone the procedure in his hospital. In all about 2,500 patients in Norway received leucotomies of one sort or another before the fashion for leucotomy began to die off in 1960s.
The approach Ødegår supported took 10 minutes, and didn’t require an operating theatre or specialist neurosurgeon. A pulse of electricity, powerful enough to cause an epileptic fit, was applied to the scalp and rendered the patient insensible. An upper eyelid was then raised and a sterile steel spike hammered through the roof of the eye socket to a depth of about 2 inches. It was then waggled from side to side, removed and the ‘operation’ repeated on the other side. In Norway this was carried out by any available surgeon and sometimes by psychiatrists. In the most careful hands the mortality from leucotomy was around 3%. In Norway 18 of the first 35 women operated on in this way died. In 1996 the Norwegian government issued a public apology to everyone who had been “leucotomised” in state hospitals and on 20th August that year allocated Kr100,000 in compensation to each survivor. In 2001, following allegations made in the newspaper Dagblat and a TV documentary, the Norwegian government appointed a commission “to investigate medical research with LSD, electrodes and radioactive rays in a vulnerable group of people without their consent”. Carl Sem-Jacobsen’s work, at Gaustad, and that of others funded by the US, formed part of that investigation. The media suggested, correctly as it turned out, that the US funded such research in Norway because they could get away with things that would have led to litigation at home. They also suggested that Sem-Jacobsen had particularly close links with the CIA, and was even a friend of William Colby, C.I.A. station head in Sweden in the early 1950s and C.I.A director from 1973-76. On the face of it the story looked promising.
+
Carl Sem-Jacobsen was awarded his medical degree in Oslo in 1941, the second year of German occupation. He was born and raised in the north of Norway, the son of an early aviator. On qualification he returned to the North to work as a doctor for a mining company and became an active member of Milorg, the Norwegian resistance movement. Milorg carried out intelligence gathering and sabotage, in collaboration with the UK’s Special Operations Executive, and also aided Norwegians who wished to escape to ‘neutral’ Sweden. Over 40,000 of his countrymen made that trip during the war. In January 1945 Sem-Jacobsen was forced to join them, his activities having been uncovered by the Gestapo.
He made his way to one of the refugee camps operated by the Swedish government, and took on the role of medical officer. American Special Forces (the fore-runner of the CIA) were active in Sweden, and particularly in those camps, gathering intelligence on occupied Norway. Sem-Jacobsen, as a member of Milorg, would have been of great interest. William Colby was a law student when the US joined the war. He volunteered for Special Forces, soldiers dropped behind enemy lines to work with resistance movements and was chosen for his first mission, in occupied France in1944, because he could speak French. Parachuted into France after D-Day he joined up with the French resistance and helped coordinate sabotage. He was chosen for his second mission because he could ski. The plan was to parachute into Northern Norway, at the beginning of 1945, along with 10 exiled Norwegians and meet up with Milorg. He would then assist with the destruction of rail links with the far North.
Finland was an ally of Germany during World War 2. When the Soviet Union invaded in force in 1944 over 100,000 German personnel escaped North to Finnmark, the most northerly Norwegian province. They then travelled south with the aim of reinforcing resistance to the allied advance in France, hence the importance of breaking the rail link. As a member of the resistance Sem-Jacobsen might well have encountered Colby, had his mission not been delayed by bad weather. In the end it was April before Colby and his men parachuted in, three months after Sem-Jacobsen flight to Sweden. Despite Sweden’s professed neutrality there was much sympathy for their neighbour, and contact with the Norwegian Government in exile. Through that link they agreed to train ‘police troops’ to cope with the immediate post-war period. Police troops were trained with weapons in secret camps and in 1945 assisted in the liberation of Finnmark and later in the rounding up of collaborators. Carl Sem-Jacobsen also worked in those camps and at the end of the war moved back into Finnmark, and continued working with former refugees. In 1950 he moved to the United States and secured a research post at the Mayo clinic in Rocester, Minnesota. He was trained in the use of EEG, the technique for recording the electrical activity of the brain from the scalp, but also became part of a pioneering research programme.
The Mayo Clinic was and is one of the USA’s foremost centres of medical excellence. It is difficult to see how a fresh Norwegian émigré with no neuroscience background would secure such a post, and not unreasonable to suggest that his work with the US Special Forces may have opened doors. The programme in which he worked involved drilling holes into the skull and inserting electrodes deep into the brain, initially in people with epilepsy. The aim was to find precise areas of abnormality, electrically overactive or unstable, that might be put out of action by coagulation. That work was soon extended to include psychiatric patients. In the1956 paper the summarized that work it is clear that he hoped to find similar abnormalities in people with psychiatric illness. From the mid 19th century many doctors overseeing mental hospitals believed that when sensitive enough tools became available, brain abnormalities would be found in people with the common and disabling mental illnesses, and some were. In 1892 Arnold Pick, a Prague psychiatrist, identified a form of dementia associated with a particular abnormality of brain cells. In 1911 Alois Alzheimer in Munich described another. In 1905 Shaudinn and Hoffman in Berlin discovered the bacteria that causes syphilis (Treponema Pallidum). The later stages of that disease were referred to as ‘general paralysis of the insane’ (G.P.I) and many infected people ended their life in an asylum. But the brains of most mentally ill patients, including those with schizophrenia and manic-depressive illness, to the naked eye and under the microscope, appeared normal. When the EEG was developed as a clinical test in the 1930s and 40s it was greeted enthusiastically by psychiatrists. It involved recording electrical signals originating from the brain from electrodes stuck to the scalp. They believed that this more dynamic test would at last reveal physical differences in the brains of people with severe mental illness. By the mid-1950s, none had been found. The work of Sem-Jacobsen at the Mayo clinic took that electrophysiological search deep into the brain, and, judging by his 1956 paper, it is clear he thought he was onto something.
Inside the frontal lobes he found small areas that produced waves of electrical pulsation slower than the surrounding brain. Viewing them as a source of abnormal ‘traffic’ within the brain his surgical colleagues destroyed them. The people to whom this was done are described as ’rather difficult, un-co-operative and incoherent active patients in great need of care’, and judged mostly improved by the operation. He goes on to describe yet another electrical change that seemed to occur when patients seemed to be hallucinating. One, for example, ‘argued rather loudly with President Eisenhower’ as seemingly aberrant waves appeared deep in their brain.
In the long run, neither observation was confirmed, but back in 1957 the visitors from England were keen to learn his technique. They also wanted the opportunity to take their own recordings from deep inside brain. Enter ‘Topsy’.
+
At the end of World War 2, hundreds of radar technicians left the RAF and joined the job market. Harold Shipton, an RAF technician had spent much of the war in South Wales developing and improving aircraft based radar. It was important work. Airborne radar enabled spotter planes to detect U-boats in the Atlantic and gave bombers early warning of fighter attacks. By the end of hostilities ‘Shippy’ had risen to Sergeant and was highly skilled in a field he likely thought had few applications in civvy street: the detection and display of weak electrical signals. However, he saw possibilities in the emerging field of bioelectrics and before demobilization visited the Burden with the aim of persuading them to take him on. Grey Walter built his first radio with his father when aged 9, an experience that kindled a life-long interest in electronics. Unfortunately his ambition sometimes outstripped his knowledge. Shipton had just the expertise he needed to realize a new idea – the toposcope, soon nicknamed ‘Topsy’. He got the job and also persuaded his new employers to take on his former assistant, Private ‘Bunny’ Warren. In 1957, before the Oslo trip, Shipton moved to a new post in Iowa.
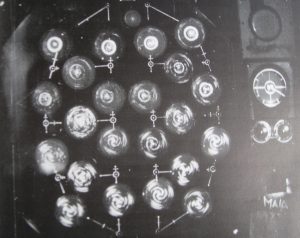
The electrical pulsations that pass through the skull from the brain are tiny, around fifty millionths of a volt. Electrodes attached to the scalp pick them up and feed them to amplifiers that boost their voltage so that they can be recorded, displayed and measured. Records where generally made, from the 1940s to the beginning of this century, by pens on moving paper. Thus rhythmic electrical pulsations, picked up by two or four electrodes back in the ‘40s, were transformed into measurable wiggly lines. The electrical signature the ‘normal’ brain had been mapped, pretty much, by the 1950s when recording from 6 or 8 electrodes became common. ‘Topsy’ was a step change. The signals from 22 electrodes were boosted and sent to 22 miniature screens: cathode ray tubes, the sort used in TVs before LEDs. Grey Walter described himself as a ‘visualist’. His idea was to create a vivid real time visual display of brain activity, the array of screens revealing electrical pulsations as they spread spreading over the surface of the brain in real time, like clouds over a planet surface.. By 1948 Shipton and Warren had created a working prototype of the ‘toposcope’. She was to undertake a range of research projects during a decade of refinements funded by the US Air Force.
The toposcope was a marvel of analogue technology, but the messages it displayed were highly complex and, in the end, amenable to only the most basic interpretation. The depth electrode studies in Oslo, and in Bristol where over 150 patients underwent such investigation and treatment, revealed little of lasting value. When digital technologies arrived in the early 1960s Topsy was abandoned; in the end, she was perhaps more much avant garde artwork than useful scientific tool and in one of his final comments on the subject Grey Walter seemed to acknowledge as much.
The mating of science and art too rarely achieves any progeny, but the strange assemblies of whirling patterns in chiaroscuro generated by our latest display systems suggests a gay pastiche of sunflowers and distant galaxies. We hope that they reflect in some way the order and beauty of vital thought.
(W Grey Walter, Preface to the 1961Penguin Edition of The Living Brain)
Sources
Ray Cooper and Jonathan Bird (1989), The Burden: Fifty years of clinical and experimental Neuroscience at the Burden Neurological Institute, White Tree Books, Bristol.
Ken Barrett, Manhandling the Brain: Psychiatric Neurosurgery in the mid-20th century, Faculty of Neuropsychiatry Newsletter, January 2016 (for more psychosurgery references). https://www.rcpsych.ac.uk/pdf/FoN_January_2016_2.pdf
Martin Walker (1993), The Cold War, Vintage, London
Grey Walter, Unpublished memoir/autobiography,
with thanks to Natasha Walter.
W.Grey Walter (1953), The Living Brain, Duckworth, London.
(1961) Penguin, London.
W.Grey Walter, R. Cooper, W.J. Aldridge, W.C. McCallum & A.L.Winter (1964), Contingent Negative Variation: An electric sign of sensori-motor association and expectancy in the Human Brain, Nature, 203, 380-384.
Randall B Woods (2013), Shadow Warrior: William Egan Colby and the CIA, Basic Books, New York,
Appendix
The Burden Neurological Clinic first opened its doors on 12th May 1939. Funded by a charitable trust it comprised wards, laboratory, library, offices and a specialist neurosurgical operating theatre. When war was declared on 3rd September that year the ‘Emergency Medical Service’ immediately requisitioned the theatre and wards to provide specialist facilities for the West Country.

The chain of events that led to the creation of ‘The Burden’ began half a century before, in Canada. In November 1891 the Rev. Harold Burden, a 32-year-old Anglican priest, and his wife Katherine, boarded a steamer bound for England. They had spent the last 3 years as missionaries to the Ojibwayo, a native Canadian tribe who lived by the great lakes. In the last 18 months Katherine had given birth to a girl and boy. Both had died within days. After their son’s demise they both became unwell and on medical advice returned to England. They were to have no more children.
On their return Harold took up a curacy in the East End of London, followed by another in Cambridge, before being appointed chaplain to Bristol prison. Continuing to work as a team, they were shocked by the home conditions of inmates, and the drunkenness of female offenders. They had found their next mission.
Their concern for ‘female inebriates’ was shared more widely at the time, and so their effort to establish specialist facilities was quickly rewarded. By the turn of the century they had created three ‘care centres’ for inebriated women, in Bristol, Norwich and Lewes. Their work also put them in touch with people judged “feeble-minded”, the next group to received the Burden’s attention.
In 1904 the UK Government set up a “Royal Commission on the Care and Control of the Feeble-Minded” in order to “consider the existing methods of dealing with idiots and epileptics, and with imbecile, feeble-minded, or defective persons not certified under the Lunacy Laws”. Harold Burden gave evidence. The commission didn’t report until 1908 and it was another five years before the “Mental Deficiency Act.” came before parliament. It recommended that the “mentally deficient” (a category that extended from the most impaired to “moral defectives”) should be taken out of asylums and workhouses and placed in specialized, licensed colonies, a proposal that mixed a more humane approach to care with a eugenic sequestration of the genetically unfit. The first person to obtain such a license was Rev. Harold Burden.
The Burdens created the “National Institutions for Person’s Requiring Care and Control” and started “Stoke Park Colony”, on the former estate of Lord Beaufort in Bristol, just north of Frenchay village. The hospital included the Dower House, an impressive four storey Georgian pile that still sits on an escarpment over looking the M32 into Bristol. Their venture was successful and within a few years they had opened two more ‘colonies’ in the area, also in redundant stately homes. When Rev. Burden died, in 1930, his estate was worth £150,000, a fortune for the time. After Katherine passed away in 1919 he had married Rosa Williams, superintendent of Stoke Park Colony and in 1933 she set up the “Burden Mental Research Trust” in Harold’s memory. The Trust funded the creation of Burden Neurological Clinic, a new build on the Stoke Park campus. ‘The Burden’ closed in the 1990s, research and clinical activities moving to the nearby Frenchay Hospital. The Burden Trust later shifted its funds to an existing neurology research group in Bristol and a housing estate built over the site of the old clinic and institute. There is no blue plaque.
MANHANDLING THE BRAIN: Psychiatric Neurosurgery in the Mid-20th Century
(The following essay is based on a talk given at the annual meeting of the Faculty of Neuropsychiatry, Royal College of Psychiatrists, on 10th September 2015. An illustrated version is available at http://www.rcpsych.ac.uk/pdf/FoN_January_2016_2.pdf )
INTRODUCTION
In the summer of 1935 the largest gathering of brain specialists in history assembled at University College, London for the 2nd World Neurological Congress. The year also marked the 100th anniversary of the birth of John Hughlings Jackson. In a profession that loves a father figure, for its’ various disciplines, Jackson was probably neurology’s. The organisers struck a medal commemorating the anniversary as a gift for delegates, asserting a kind of British precedence at the outset.
The programme was wide ranging:
The Epilepsies included some of the earliest EEG studies in people with epilepsy.
The Frontal Lobes, a whole day session, included an overview by Kurt Goldstein, a brain injury specialist en-route to the USA, having been expelled from Germany by the Nazis. There were sessions on the CSF and hypothalamus, and 250 ‘free’ presentations, but the star of the show was undoubtedly an 86-year-old Russian: Ivan Pavlov. Pavlov was awarded his Nobel Prize at the turn of the century for meticulous work on gastric physiology, which was followed by his seminal studies on conditioning in dogs. An editorial in The Lancet the following week noted:
‘In these researches we discern not only elaborate care in design and execution, but the perfection of a new experimental method – a method whose conception signifies genius.’1
In his last decade (he died six months after the Congress) Pavlov’s new interest was psychiatry. The Soviets opened a psychiatric clinic next to his laboratory and on Wednesdays he gave his opinion on clinical cases. His London lecture, “delivered to a packed hall” (so reported the New York Times) summarised his thoughts on the subject. The Lancet also reported that Pavlov was made an Honorary Member of the Royal Society of Medicine who hosted a drinks reception on the Friday, followed by ‘a cinema entertainment’. They don’t tell us the film but there were several hits that summer. Werewolf of London, would have been ideal. A scientist, savaged by a beast on a field trip, returns to London and, at the first full moon, transforms into a werewolf. Cultural historians like to read ‘horror’ movies as metaphors for their time. In 1935 the most dangerous ‘beast’ at large in the world was ideas. Communism, Fascism and National Socialism were about to wipe out tens of millions of people, and during that congress an idea would take hold of a member of the organizing committee. In consequence, almost as many people would die as on 9:11, three times that number would be rendered epileptic, and over 70,000 brain damaged. That idea was “prefrontal leucotomy”.
When I trained in the late 1970s leucotomy had come to epitomize psychiatry at its most oppressive and controlling, an object lesson in the medical hubris. So why revisit it now? In the last two decades a number of scholarly publications have shed new light on the leucotomy story and the context in which it occurred. But there is a more pressing reason. By the 1980s electrodes could be accurately placed in the brain and left in situ along with an electrical stimulator. “Deep Brain Stimulation” (DBS) or “neuromodulation” has since been used to treat hundreds of patients with movement disorders. In 1999 workers in Belgium suggested it might help people with other intractable conditions, including Tourette’s, OCD and depression. Five years on a neurologist wrote:
‘Now that Deep Brain Stimulation means the surgery is reversible, we no longer have to worry about permanent harm…On the other hand, now that psychosurgery could be readily available, potentially for a large number of conditions, we have a lot more to worry about.’2
Since then trials of DBS have extended to include people with PTSD, anorexia, obesity and substance misuse. There is even talk of enhancing ‘normal’ functioning with the technique and 2014 saw the publication of the first book with the word ‘”psychosurgery” in the title for 40 years. If we know anything about humans it is that we tend to repeat our mistakes. Perhaps now is the time to revisit that first wave of psychosurgery, in the middle of the last century, to try and understand how so many of our colleagues were willing to damage their patients in the name of “treatment”. What follows catalogues the main events but also attempts to get to know some of the key players, and to understand something of their world and thought.
HOW DID IT HAPPEN?
In the 1930s an oxide of thorium, marketed under the name Thorotrast, was found to be radio-opaque and became popular as an X-ray contrast medium. Several studies presented at the 1935 congress employed it, including four from the world’s leading brain angiography department, headed by the professor of neurology in Lisbon, Egas Moniz. Moniz qualified in medicine at the turn of the century then studied neurology in Paris under Marie and Babinski. Back in Portugal he obtained an academic post but also got elected to parliament and during World War 1, when Portugal was neutral, he joined the cabinet and rose to be Foreign Secretary. In the 1920s Portuguese politics veered to the right and eventually dictatorship. Thereafter Moniz focused on his academic career visiting Paris briefly to find a subject to study. X-ray imaging of the ventricles and spinal cord were possible at that time but no one had been able to reveal the blood vessels of the brain. In 1927, after a year of experimentation on dogs and cadavers, Moniz produced the first cerebral angiogram and headed back to Paris to claim precedence. For the next 20 years angiography was his main interest and his department conducted over 200 studies. Several were presented at the Congress, including a whole wall of posters.
Thorotrast was also of interest to a doctor and academic from Washington DC called Walter Freeman. He had persuaded neurosurgical colleagues to use the medium instead of air in a series of ventriculograms and took a presentation to London. The organizers placed his more modest poster alongside the Portuguese group. Freeman and Moniz met and got on well, conversing in French. Freeman had also studied neurology in Paris, in the 1920s before his influential grandfather secured him a post in Washington. He was to run a new pathology department at St Elizabeth’s, a 3000 bed state mental hospital. Over the next decade he performed over 1000 post mortems, published papers and a textbook on neuropathology and lectured at the local university.
But Moniz and Freeman had another thing in common: neurology private practice. Writing of the 1930s Elliot Slater, a leading English psychiatrist, noted that, at that time “neurologists monopolised the large and lucrative practice to be derived from neurotic and mentally disturbed patients”.3 The mentally ill with money evidently preferred neurologists to asylum doctors. Slater goes on to say that patients would receive a thorough physical, be reassured there was no ‘real’ illness, and then be sent back to their GP for bromide. Moniz however worked in a private clinic that boasted a range of electrical therapies (this was before the convulsive variety), which he employed liberally on his psychiatric cases. But he wanted to do more, particularly for those stuck in the rut of late life depression, chronic anxiety and obsessionality. Citing Pavlov and the anatomist Cajal as influences, he pondered the neural basis of those symptoms. It was well known that the brains of such patients were usually normal in structure so he toyed with a new paradigm to explain their problems. “The cellular bodies remain altogether normal…but their multiple liaisons, very variable in normal people…have arrangements that are more or less fixed, resulting in persistent ideas and deliria”. That being the case, it may be possible to “suppress certain psychological complexes by destroying the cell connected groups” a development that would be “a great step forward”4. In his view the most likely location for those over-connected pathways was the tracts between prefrontal cortex and the thalamus.
At the London Congress Moniz and Freeman attended the day of lectures on the frontal lobes, and a later session on physiology in which Jacobson, from Yale, presented the mixed results of removing the frontal lobes from monkeys (one was became calm, the other agitated). Looking back Moniz was unable to say exactly when he decided to turn his speculations into practice but on his return to Lisbon he wasted little time. Almeida Lima, a young neurosurgeon who had accompanied him to London, was recruited along with the local professor of psychiatry and on 12th November 1935 Moniz and Lima performed the first prefrontal leucotomy. Their patient, ‘MC’, was a woman of 63 who had been in hospital for three years with to a mix of depression, anxiety and paranoia. Under general anaesthetic, and directed by Moniz, Lima made boreholes in the top of her skull, inserted a long needle down to the base of the frontal lobes and injected a small amount of pure ethanol (a substance commonly used to destroy nerves as a treatment for neuralgia) at three points in each hemisphere.
The patient survived the procedure and, in Moniz’s opinion the effect on her mental state was positive. He therefore embarked on a series of twenty but along the way he became concerned at the unpredictability of the alcohol method and so devised a surgical instrument, his ‘leucotome’ or ‘corer, essentially a hollow spike out of which a small loop of wire could be pushed and rotated.
The twenty were all long-term inpatients, none died and, again in his view, no one was worse. Ten with ‘agitated melancholia’ or ‘acute anxiety’ were judged ‘recovered or improved’ as were four others diagnosed as schizophrenic or manic. That results prompted him to carry out another series but before that he wrote a paper in French on the first group and sent a junior colleague to a neurological meeting in Paris to present it. Moniz was highly regarded in the city but it was not well received. One comment was typical: “Malaria therapy, insulin therapy…were inspired by clinical findings…By contrast, no-one has ever seen an organ improve its function after a hazardous mutilation”5. More damning was the view of Sobral Cid, the professor of psychiatry who had provided the first patients. He had been unhappy with their condition on return to his care and after the first 4 refused to cooperate. Following pressure from Moniz he agreed to continue but after 15 called a halt and the neurologist was forced to go to another hospital for the remaining five and the next series of 21. Cid did not agree with Moniz’s view of the outcomes and called his speculation on the neural basis of the symptoms nothing more than ‘cerebral mythology’.
Undeterred, Moniz had his paper translated into several languages including Spanish and Italian and the procedure was soon copied in Cuba, Brazil, Rumania and, with most enthusiasm, Italy. Moniz accepted a free two-week holiday in the country to demonstrate the technique. Italy was perhaps particularly receptive because at that time neurology and psychiatry were part of a single medical discipline and in little more than a year over a hundred leucotomies had been performed, including some with improvisation. At the time the only truly effective treatment in psychiatry was infection with malaria to treat neurosyphilis. One Italian thought it might be best delivered directly into the brain and used a trocar to punch a hole through the orbital bone, entering under an eyelid. The technique didn’t catch on but a neuropsychiatrist called Fiamberti adopted it, rather than bore-holes, to inject alcohol into the frontal lobes.
Moniz expanded his paper into a 250-page monograph, “Tentative operatories dans le traitement de certaines psychoses” and having recently heard from his new American friend, Walter Freeman, sent him an autographed copy. Freeman was impressed. He had recently recruited a neurosurgeon, James Watts, to teach with him, and suggested they might carry out their own series. Watts was interested in part because he had spent time at Yale in Fulton’s physiology laboratory, where experiments on the frontal lobes of monkeys were carried out. But Freeman wasn’t a psychiatrist and his own hospital, St Elizabeth’s, refused to cooperate so he looked elsewhere for patients. They began their series with a Moniz leucotome but soon adopted their own technique (entering the brain through a hole in the temporal bones with a blunt knife which was then swept up and down to sever the tracts). There were no deaths in their first series of twenty and Freeman noted that worry and anxiety in particular were markedly reduced in their patients. They presented the work at a series of psychiatric meetings and the response was often highly critical:
“As a pathologist he may not have much fear of looping out pieces of sub-cortical tissue…”
“This is not an operation but a mutilation”.
“You are burning down a house to roast a pig”.6
The last was from Smith Ely Jelliffe, a leading psychoanalyst. In his defence Freeman insisted that ‘a brain can take a good deal of manhandling’.
Their first presentation, however, was in Baltimore before the patient series was complete, at a meeting attended by Adolph Meyer, an influential figure in American psychiatry. Meyer promoted the notion of psychiatric ‘disorder’ rather than disease, was not much interested in traditional diagnostic labelling and viewed psychiatric ‘illness’ as reaction to the individual’s environment. Leucotomy was not aimed at specific diagnoses but at modifying affective response. Meyer concluded, “…the available facts are sufficient to justify the procedure in the hands of responsible persons” . Kurt Goldstein, the recent German émigré and brain injury specialist also attended one of the meetings but had also spoken to some of Freeman’s patients.
‘What some of the patients have told me about their condition before and after the operation was impressive…the affective attitude seemed to have changed completely…which the patients particularly appreciated’.7
In writing up the series Freeman and Watts concluded, cautiously that “…the indiscriminate use of this procedure would result in vast harm….it should be reserved for a small group of specially selected cases…” 6 But some psychiatrists didn’t agree that the reach of the technique should be so limited. In order to understand why you need to know something of US psychiatry at that time, and in particular how it was practiced in large state mental institutions. A case in point is Pilgrim State Hospital on Long Island New York.
The hospital was built in the early 1930s and aimed to be state of the art. It had 10,000 beds, which was not uncommon in the US, but was proud of its standards of care and the speed with which it introduced new therapies (malaria, insulin coma etc..). Less wealthy states were not so fortunate. During World War Two many conscientious objectors were sent to work in state mental hospital and witnessed very poor standards of care. Some collected evidence and at war end a group in Ohio approached a leading churchman who in turn went to the State Governor. An article in Life magazine entitled ‘Bedlam 1946’ exposed shockingly poor standards and included photographs of naked and soiled patients standing idle (echoing images from the holocaust). The resulting scandal led to an increase in mental health funding in many states in the late 1940s.
The fact was that if a patient remained in a state mental institution for two years there was very little chance of discharge. Imagine for a moment the most disturbed 5% of inpatients (500 at Pilgrim State) at a time when the only effective treatments were malaria and sedation. If there was any possibility that a new technique might modify behaviour (in addition to muting emotional response) it was, surely, worth a try. Their relatives were likely to seize any chance of improvement and what, in the end, did the patient have to loose? When the techniques was tried, in that context, previously unmanageable behaviours were often diminished or eliminated, patients were able to move from disturbed to open wards, and some were discharged altogether.
Surgeons at this time were often portrayed in the press as heroic figures working at the frontiers of medicine, and this was a case in point. Overblown stories with vivid headlines began to appear. “Wizardry of surgery restores sanity to fifty raving maniacs” trumpeted one newspaper. Leucotomy gradually took off as a potent way of modifying behaviour and Freeman was quick to shed his earlier caution. When he and Watts produced the first textbook on psychosurgery in 1942 the book jacket announced that “those treasured frontal lobes, supposedly man’s most precious possession, can bring him to psychosis and suicide…” and that the book revealed how “…personality can be cut to measure, sounding a note of hope for those who are afflicted with insanity”. Elsewhere he claimed they were producing a “surgically induced childhood”, a comment that was particularly inspired. Having taken the ill person back to childhood, who better to help them reconstruct their ego than psychoanalysts, earlier opponents of the procedure?
BUT HOW COULD THEY DO THAT?
By the summer of 1940 no leucotomies had been carried out in Britain, and the country had been at war with Germany for a year. In the months before the war William Sargant, a recently qualified Maudsley Hospital psychiatrist, went on a study tour of the USA where he met Walter Freeman and interviewed several of his patients. He returned eager to use the treatment in Britain but the Maudsley refused to allow their patients to be surgically brain damaged. Undeterred, Sargant contacted an old teacher, Professor Frederick Golla. He is an important figure in this story and so we will look at his career in some detail.
Golla trained in neurology at Queen’s Square at the beginning of the 20th century, the final years of Hughling Jackson’s working life. He was then appointed assistant physician at their Maida Vale branch, went into private-practice and was set for a conventional career in neurology had the First World War not intervened. He volunteered, saw action in France and became intrigued by soldiers’ reaction to combat. He took a particular interest in ‘shell shock’ and came to believe that he could predict who in his company would break down. He later served on War Office committees where he met Sir Frederick Mott, the founder of the Maudsley Hospital and an authority on ‘battle neurosis’. After the war Golla returned to his neurology practice but also began a series of experiments, at the Maudsley’s Central Pathology laboratory (which was directed by Mott) looking for physiological markers of vulnerability to neurosis. His approach was in many ways the opposite of Pavlov’s; he flitted from one technique to another without coming to firm conclusions, but the work was innovative and Mott was impressed. In 1921 Golla was invited to give the prestigious Croonian Lectures, which he titled “The objective study of neurosis”.
In addition to directing his laboratory Mott was also responsible for coordinating psychiatric training and research in London and when he retired in 1924 Golla was appointed, on his recommendation, as his successor. In modern parlance Golla was a ‘behavioural’ neurologist who maintained a strictly constitutional/organic view of mental illness and had little sympathy for the growing popularity of psychological therapies. In 1938 he was appointed Professor of Mental Pathology at London University and was also headhunted for a new post: directorship of the newly created Burden Neurological Clinic, in Bristol.
The ‘Burden’ was set up by a charitable trust for “the cure elimination amelioration study or investigation…into ailments diseases or other matters of a cerebral or nervous nature…including mental disorder and mental defect”.8 Golla was invited to put together a clinical and research team and in 1939, at the age of 60, took the job. The following year he appointed his clinical director, Effie Hutton, a London psychiatrist with a track record of research.
When Sargant contacted Golla in 1940 regarding the possibility of beginning a leucotomy trial in the UK he was enthusiastic and passed the job of selecting patients, and publishing the results, to Effie Hutton. The first such patient, ‘VB’, underwent leucotomy on 19th February 1941.
Bristol was a major port with a large aircraft factory and a prime target for German bombing. Raids began in August 1940 and continued until the following April, killing over 1200 people. After each raid a band of labourers cleared the rubble and ‘VB’ was one of them. During a daylight raid in the autumn an occupied bomb shelter was hit and VB, a veteran of the trenches, helped with the clear up. He had returned from the First War relatively unscathed, physically. He married and started a family, but before long nightmares began, followed by bouts of anxiety and depression and gradual social withdrawal. He was unable to work for long periods but by 1940 was employed again and holding it together, until that shelter was hit. After the clean up he was unable to sleep or eat for several days and thereafter wandered the street in a state of anxiety listening for air raid sirens, and feeling a coward as his wife and children seemed unconcerned. He eventually saw a psychiatrist who told him of a new surgical treatment had recently arrived from the US and was only available in Bristol.
Effie Hutton admitted VB to the Burden on 15th February 1941 and four days later a frontal leucotomy was performed, using the Watts and Freeman technique, under local anaesthetic. In the absence of a ‘leucotome’, the surgeon improvised with a paper knife. Frederick Golla observed the procedure and later wrote that VB was
‘… talking the whole time and when the severance of the tracts took place the talking continued without the least hiatus or any indication that anything had happened.’ 9
Immediately after the operation his nightmares stopped and he was no longer anxious. Though there were several air raids during his stay in hospital he was untroubled by them and when discharged two months later he returned to work as a labourer. Golla concluded:
‘Until such time as we realize the almost infinite lability of the CNS…we shall…find ourselves outwitted by the recuperative powers of the damaged nervous system’.
He goes on to say that the brain is not fixed like a telephone exchange, but is adaptable, citing a personal experience in support. Whilst training in neurology at Queen’s Square he assisted Sir Victor Horlsey, Britain’s first specialist neurosurgeon, in an operation for Jacksonian epilepsy. (This was around 1906; remarkably, Horsley had performed his first successful operations for Jacksonian seizures, 20 years before). Seizures began in the patient’s thumb then spread to his hand and arm. The operation, which involved removal of the hand area of the motor cortex, cured the epilepsy and left the patient with flaccid paralysis of the hand. But over the following months the hand regained movement and power and a year later his only complaint was about his tennis swing. His brain had compensated for the surgical damage.
Belief in the adaptability of the brain was part of a mid-20th-century debate on brain function that had it’s origin in the 19th century. In 1874 Hughlings Jackson wrote:
‘To locate the damage which destroys speech and to locate speech are two different things’. 10
He agreed with Broca that damage to an area of the left frontal lobe impaired speech production but disagreed that speech, and other functions, were so strictly ‘localised’. Over the next 30 years, as more functions became mapped onto the cortex, medical opinion moved away from Jackson’s view, but at the beginning of the 20th century the tide began to turn. Pierre Marie, the leading Paris neurologist, examined the preserved brain of Broca’s key patient and arrived at different conclusions. The First World War produced unprecedented numbers of young men with focal brain damage. Henry Head in the UK and Kurt Goldstein in Germany took a particular interest in their treatment and rehabilitation. They concluded that the remarkable levels of recovery reached by many were simply incompatible with an entirely fixed, immutable, localisation of function. Lashley in the US and von Monakow in Switzerland held similar views and so evolved a more dynamic, holistic view of the brain, a view clearly shared by Golla, Freeman and Moniz. If the brain had the capacity to adapt, so went the argument, it was worth making it do so in cases of severe intractable mental illness.
In July 1941 the Lancet published a paper by Effie Hutton describing the first eight patients treated with leucotomy at the Burden. Thereafter, the technique was widely adopted in the UK. As the war drew to a close the body responsible for psychiatric hospitals, the ‘Board of Control’, decided to find out just widely and with what effect. Printed cards were sent out listing age, sex, diagnosis and outcome and hospitals were required to complete and return them on all patients who had the operation. The numbers were impressive and in 1947 they finally published their analysis, a 30-page document entitled “Prefrontal Leucotomy in 1000 Cases”. The document concluded that a third of the people treated had resumed their everyday activities “without that emotional tension and preoccupation with hallucinations and phantasies which has hitherto handicapped them”. Women outnumbered men by a ratio of 3 to 2 (a remarkably constant finding, internationally). The operative death rate (from haemorrhage) was around 3%, post-operative epilepsy 10%. Also listed were a range of adverse effects of variable severity and duration, including urinary incontinence, disinhibition, impaired drive and initiative, insight and foresight. Standard tests of intelligence where however generally unimpaired. It is a remarkable document, not as a reliable guide to the efficacy of the treatment but as a snapshot of clinicians’ opinion. For example, a histogram illustrates a range of symptoms, and how many were judged ‘gone’ after treatment. They included agitation (71.3%), depression (71%), obsession (53.1%) and delusion (36.6%). In light of that the Board of Control supported continued use of leucotomy.
I found the report difficult to get hold of and eventually read it in the Public Records Office. The relevant government file included a hand-written follow up note prepared in response to an MP’s question in the early 1950s, on the extent of the practice. In five years from 1948 to 1952 there were 7225 operations of which 4468 were on women. There were 169 operative deaths.
WHY DID IT FALL OUT OF FAVOUR?
When the World War ended in 1945, Walter Freeman’s reputation was in some respects riding high. The treatment he had promoted and modified was being used to relieve hundreds of mentally ill patients. Thanks to him the technique had been adopted enthusiastically in Britain and Scandinavia (Sweden was to become the most leucotomised nation in the world) and he was the co-author of the first textbook on the subject. But for him the procedure had one major drawback: cost. Each operation cost around 500 dollars and many poorer states were unable or unwilling to spend that amount on a single patient. As a result thousands of people who might have been helped by ‘lobotomy’ (his preferred term) languished in state mental hospitals with little hope. A simpler and less expensive technique was required and by the end of that year he believed he had found it, by combining two Italian innovations: electroconvulsive therapy and a ‘trans-orbital’ approach.
By 1945 Freeman was using unmodified ECT (i.e. without general anaesthetic or a muscle relaxant) as an outpatient, office procedure. He noted that when two applications were given, one immediately after the other, the patient was rendered unconscious for several minutes. Since1937 Fiamberti in Italy had continued injecting alcohol into the frontal lobes via holes punched through the orbit, above the eyes. Freeman’s idea was to render the patient unconscious with ECT and then insert a suitably sharp instrument under the upper eyelid, through the orbital bones and into the frontal lobes. Sweeping the instrument sideways could then sever the white matter tracts. He reasoned that as tears were sterile operating theatre conditions were not required. After experimenting on cadavers with a range of sharp objects he eventually found the solutions in his kitchen drawer: the ice pick.
By January 1946 he had chosen his first subject, a 29-year-old woman with recurrent agitated depression, one of his private outpatients. Whilst her husband and 4-year-old daughter waited in the waiting room, Freeman gave two applications of ECT, raised an upper eyelid and, using a hammer, punched a sterilised ice-pick 7cm into her brain. He then swept the handle sideways over the nose before removing it. In his diary he recorded that he had been overcautious on that first occasion and so only treated one side. He got her back the following week and repeated the procedure on the other.
The patent suffered black eyes and short periods of confusion but her depression remitted and she later to bought Freeman an expensive watch, as a token of her thanks. Freeman was encouraged to continue, but it was some months before he shared the fact with colleagues who, in the event, strongly advised him to stop. He didn’t, but replaced the ice-pick with a pair of self-designed ‘leucotomes’ and over the next twenty years promoted the technique at home and abroad. He operated on many patients, often in previously neglected backwaters of the country and was to boast that he needed only 6 minutes per procedure. It is estimated that he performed over 3000, including around twenty on patients under the age of 18. In 1967a patient on whom he had already performed two such operations relapsed and asked him for third. He obliged, she died of a brain haemorrhage and when the details became known his hospital refused to let him perform any more. By that time his reputation had already been damaged, and as the years progressed he was increasingly vilified.
In 1947 neurosurgical facilities moved out of the Burden Neurological Clinic and into nearby Frenchay Hospital. This was probably a relief to Effie Hutton; she had become increasingly concerned about the side effects of leucotomy and published a series of papers on the subject in the late ‘40s. One included a six-year follow up of that first patient, ‘VB’. Though he continued to regard leucotomy as ‘the best thing that has every happened’ to him those close to him disagreed. He hadn’t remained in work for long, as he was unreliable. He refused to take a bath, was often foul-mouthed, irritable and, in his wife’s words, ‘impossible to live with’.
1947 also saw the first conference on the frontal lobes, this time in New York, and including a session on leucotomy. Moniz’s ‘cerebral mythology’, the desirability of interrupting the connection between the prefrontal area and thalamus, was not seriously challenged, but adverse effects and how to avoid them took centre stage. Over subsequent years surgeons sought maximum benefit from minimum destruction, targets including the prefrontal cortex (topectemy) the white matter (capsulotomy and subcaudate tractotomy and others) and medial thalamotomy. The latter is of interest because a neurologist and surgeon invented a ‘stereotactic cage’ to find it, the first time this type of surgery had been used in humans. Other surgeons, including Hugh Cairns in the UK, targeted limbic structures, including the cingulate gyrus. In 1948 Lisbon hosted the first international conference on psychosurgery, with presentations from 14 countries, and the following year Moniz shared the Nobel Prize for medicine, awarded for leucotomy rather than angiography.
Despite technical innovations the number of operations performed declined through the 1950s. The dramatic improvements previously reported by clinicians, as recorded in the Board of Control report, became more elusive as the eye of faith was replaced by more objective methods of assessment, and longer-term follow-up. However, the main reason for the decline was almost certainly the introduction, in 1952, of Chlorpromazine. In those early days the drug was even marketed as a chemical alternative to leucotomy. In the 1960s aggressive and other ‘undesirable’ behaviours in adults and children were targeted by psychosurgeons, particularly in India and Japan. Such developments helped fuel an ethical debate that lead to much stricter control and regulation, but not, in most countries, an outright ban. In truth, psychosurgery never went away.
CONCLUSION
Thirty years ago I was fortunate to spend three months as a visiting fellow in behavioural neurology in Boston, Mass.. One afternoon, at the suggestion of a colleague, I travelled across town to meet a neurosurgeon called Tom Ballantine. He was emeritus professor of neurosurgery at Harvard and as a lowly senior registrar I felt somewhat intimidated. I needn’t have: he was warm, welcoming and pleased to talk about his work, especially with a psychiatrist. He had just written up a series of almost 200 cingulotomy operations, performed for treatment resistant depression or intractable pain. I was impressed by and commented on the number of psychiatric textbooks on his bookshelf. He was at pains to reassure me that he didn’t do his own psychiatric assessments, they had a psychiatrist on the team for that, but he felt he needed to understand the language and issues. His team also included a psychologist and ethicist . I mention the visit not to promote cingulotomy, but because I believe Ballantine’s approach contains useful lessons.
Firstly I don’t believe he, or any neurosurgeon I have met, would have said the brain ‘can take a good deal of manhandling’. It can’t and is best protected by keeping psychiatrists, neurologists and pathologists well away from it, at least in life.
The second point is about teams and their hierarchies. Despite his status, physical size (he was tall), and white coat, Ballantine was warm and open. It is fairly well known that key decisions on the flight deck of commercial aircrafts are now made collaboratively. The hierarchy was flattened as a result of fatal accident enquiries. The same is true of psychosurgical teams; though one should never underestimate the power of a senior doctor with a bee in his bonnet.
The final point takes us back to Pavlov and his methodical, controlled and exhaustive approach to research. In an afterword to the 2014 textbook on psychosurgery mentioned earlier, Marwan Hariz, Professor of Functional Neurosurgery at Queen’s Square, noted:
‘Since 1999… there have been eight published targets for DBS in OCD, ten in Tourette, nine depression…Despite this lack of consensus…DBS is now being trialed for drug addiction, anorexia nervosa, PTSD, dementias, and…for enhancement of cognition in normal people’.11
With so many disorders to choose from, and so many possible targets to ‘neuromodulate’, the likelihood of accumulating a large series of patients, followed up long-term and focusing on a single site and disorder, seems remote. That approach certainly wasn’t adopted before leucotomy took off in the middle of the last century, and in this essay I have explored some of the reasons why. Those reasons no longer apply.
Acknowledgement:
I’m grateful for the assistance of Jane Sweetland, librarian at Southmead Hospital Bristol, Jackie Cheshire at the Rockefeller Library, Institute of Neurology, and the library of the Royal Society of Medicine. The photographs of Pavlov, Moniz and Freeman are, to the best of my knowledge, open source. Those of Golla and Hutton were courtesy of Ray Cooper. The paper knife and stamp are from my own collection.
REFERENCES
- Pavlov, Annotation, Lancet, August 3, 1935, 258.
- Marc Leveque (2014), Psychosurgery: New Techniques for Brain Disorders, Springer, p.324.
- Slater E (1975), Psychiatry in the Thirties, Contemporary Review, 226, 70-5
- Kotowicz Z (2012), Psychosurgery: the Birth of a New Scientific Paradigm, Centre for Philosophy of Science, University of Lisbon, p.56.
- , p.98.
- Pressman JD (1998), Last Resort: Psychosurgery and the Limits of Medicine, Cambridge University Press, p. 80.
- Ibid, p. 83.
- Cooper R and Bird J (1989), The Burden: Fifty years of clinical and experimental neuroscience at the Burden Neurological Institute, White Tree Books, p. 1
- Golla F L,(1943), The Range and Technique of Prefrontal Leucotomy, Journal of Mental Science, 89; 189-191.
- Jackson J H, On the Nature of the Duality of the Brain, in Selected Writings of John Hughlings Jackson, Volume 2, James Taylor et al, Eds. 129-125, Hodder and Stoughton, London, 1932, p.130.
- Leveque M (2014), Psychosurgery: New Techniques for Brain Disorders, Springer, p. 323.
BIBLIOGRAPHY
Psychosurgery:
Moniz E (1936), Tentatives operatoires dans le traitement de certaines psychoses, Masson, Paris.
Freeman W, Watts JW & Hunt T (1942) Psychosurgery: Intelligence, emotion and social behavior following prefrontal lobotomy for mental disorders. Springfield, Thomas.
Board of Control (1947), Pre-frontal Leucotomy in 1000 Cases, HMSO.
Shutts D (1982), Lobotomy: Resort to the Knife, Van Nostrand Reinhold, New York.
Rylander G ( 1948), Personality Analysis Before and After Frontal Lobotomy, in The Frontal Lobes , John F Fulton et al Eds., pp691-705. Williams and Wilkins, Baltimore.
Vallenstein ES (1986), Great and Desperate Cures: The Rise and Decline of Psychosurgery and Other Radical treatments for Mental Illness, Basic Books Inc..
Pressman JD, Last Resort: Psychosurgery and the Limits of Medicine, Cambridge University Press, 1998.
El-Hai J (2005), The Lobotomist: A Maverick Medical Genius and His Tragic Quest to Rid the World of Mental Illness, John Wiley & Sons.
Howard Dully and Charles Fleming, Messing with my Head: The shocking true story of my lobotomy, Vermilion, 2007.
Kotowicz Z (2012), Psychosurgery: the Birth of a New Scientific Paradigm, Centre for Philosophy of Science, University of Lisbon.
Raz M (2013), The Lobotomy Letters: The Making of American Psychosurgery , University of Rochester Press.
Other topics:
Goldstein K (1935), The Organism, Zone Books, NY, 1995.
Harrington A (1987), Medicine, Mind and the Double Brain, Princeton University Press.
Ferone G & Vincent J-D (2011), Bienvenue en Transhumanie: sur l’homme de demain, Editions Grasset & Fasquelle, Paris.
Todes DP (2014), Ivan Pavlov: A Russian Life in Science, Oxford University Press.
Comment: I found Last Resort the most balanced and rewarding in the list. It includes a good account of the psychiatric environment at that time. The Lobotomy Letters, contains an interesting discussion on holism, the history of which is covered in Medicine, Mind and the Double Brain. Psychosurgery: the Birth of a New Scientific Paradigm has the most detailed account of Moniz (it is by a Portuguese academic), and has a fascinating chapter on Phineus Gage. The recent Pavlov biography is large, but interesting on neuropsychiatry in Russia at the turn of the century, and much else.
OTHER SOURCES
Horsley V (1909), The Function of the So-called Motor area of the Brain, BMJ, 2(2533) July 17, 121-132.
International Neurological Congress, Lancet, August 3, 1935, 268-269; August 10, 332-336.
Freeman, W. J., & Watts, J. W. (1937). Prefrontal lobotomy in the treatment of mental disorders. Southern Medical Journal, 30, 23–31.
Hutton E L (1941), Early Results of Prefrontal Leucotomy, Lancet, July 5, 3-12.
Hutton E L (1942), The Investigation of Personality in Patients treated by Prefrontal Leucotomy, Journal of Mental Science, 371, 275-281.
Golla F L,(1943), The Range and Technique of Prefrontal Leucotomy, Journal of Mental Science, 89; 189-191.
Maisel A Q, Bedlam 1946, Life, 6 May 1946, 102-118
(available online at 4.10.15: https://books.google.co.uk/books?id=BlUEAAAAMBAJ&q=maisel#v=snippet&q=maisel&f=false)
Hutton E L, (1947) Contra-indications for Leucotomy: Whom Not To Leucotomise, Journal of Mental Science, 93:337-341.
Hutton E L, (1948) The Effect of Leucotomy on Creative Personality, Journal of Mental Science, 94, 230-235.
Freeman F (1948), Transorbital Leucotomy, Lancet, Sept 4, 371-373.
Taylor D C (1986), One hundred years of epilepsy surgery: Sir Victor Horsley’s contribution, J Neurol Neurosurg Psychiatry, 49(5): 485–488.
The songs of George Formby: An analysis
In 1943 the writer George Orwell published an essay on Donald McGill, the foremost ’saucy postcard’ artist of the interwar years. The essay contains an unsurpassed analysis of the content of such postcards and discusses their public appeal:
Their existence, and the fact that people want them, is symptomatically important. Like the music halls, they are a sort of saturnalia, a harmless rebellion against virtue. They express only one tendency in the human mind, but a tendency which is always there and will find its outlet, like water. On the whole, human beings want to be good, but not too good, and not quite all the time. [1]
In this essay I will apply Orwell’s method to an analysis of the songs of a performer from the music hall tradition: George Formby.
Formby’s comic persona, a gormless and naïve working class chap from Lancashire, was hugely popular with the British public. His films and records made him the highest paid family entertainer in Britain in the late 1930s and during the World War 2[2]. In common with the music hall tradition, most of his songs contain frequent sexual innuendo.
’When I’m cleaning windows’ [3], undoubtedly his most popular song, featured in the 1937 film ‘Keep Your Seats Please’ and was banned by the BBC because of its content. Such was its popularity that Formby or his collaborators wrote a sequel the following year. Of the 12 verses in the two versions 9 contain sexual references as follows:
- The sexual activities of newly-weds (3 verses)
- Women undressing (2 verses)
- Naked women (2 verses)
- Sexually frustrated ‘old maid’ (1 verse)
- His large penis (1 verse)
These parallel the themes of McGill’s art, but in addition, the song is sung from the point of view of a seasoned voyeur who has no doubt that ‘a window cleaner you would be’ if you could witness the above. One verse begins with the line ‘Pajamas lying side by side’. Orwell observed that homosexuality never featured in McGill’s postcards[4], but there seems no other reason to mention such a thing, other than for its gay (and at the time highly salacious) implication.
A line of dialogue that features in more than one Formby films, addressed to the attractive female lead, is ’you’d look good with nothing on’.[5] Where such a line to be delivered by comedians such as Sid James or Max Miller their macho personas would have made it course. Formby’s character delivers it in a voice that is just this side of camp, the voice of a wet mummy’s boy, and it is usually followed by an embarrassed ‘oh no, I didn’t mean…”. In consequence, we believe it was a gaff and laugh at George rather than with him. He employed the same voice for most of his songs and this perhaps rendered them almost innocent. It also makes the voyeuristic persona of ‘window cleaner’ creepily believable.
A comic device that does not feature in that song is word substitution, as in the following example from ‘Chinese Laundry Blues’:
‘Now Mr Wu, has got a naughty eye that flickers,
You ought to see it wobble when he’s ironing lady’s…blouses’. [6]
‘Aunty Maggie’s Remedy’ employs the same effect to underscore the risqué content:
Now I know a girl, who is putting on weight,
In a spot where it just shouldn’t be
So I said to Nelly‘Now you rub your…ankle
With Aunty Maggie’s remedy. [7]
In the song ‘With My Little Stick of Blackpool Rock’ the very subject (a long, cylindrical pink object) suggests a double meaning that is reinforced by such lines as:
In my pocket it got stuck I could tell,
For when I pulled it out I pulled my shirt out as well.[8]
The song also includes a particularly bizarre verse in which are told of a drowning girl who asks the singer to save her only to be told ‘ well if you’re drowning then I don’t want to loose, my little stick of Blackpool Rock’. The tendency to underscore double meaning also features in ‘Little Ukulele’[9], a song in which the true meaning, the virtues of holding onto one’s penis, is particularly thinly veiled. Early in the song we learn that his mother had advised the singer ‘do what I say, and you’ll never go astray, if you keep your ukulele in your hand’, good advice, perhaps, given the shame of unwanted pregnancy and the fact that venereal disease was untreatable at the time. In second verse in he describes sitting by the sea with a girl:
I felt so shy and bashful sitting there
For the things she said I didn’t understand
She said your love just turns me dizzy
So come on big boy get busy,
But I kept my ukulele in my hand.
Formby returned to the voyeur theme with ‘In my little snapshot album’ [10] in which we are told of a camera that can ‘take pictures in the dark and even see through brick’. The resulting photographs, of the unspecified sexual activity of neighbours and family, are stored in the album of the title. The song ends on a theme more than once depicted by McGill.
I’ve got a picture of a nudist camp…
All very jolly tho’ a trifle damp…
There’s Uncle Dick without a care
Discarding all his underwear,
But his watch and chain still dangle there
In my little snapshot album.
Whilst a majority of Formby’s songs have a risqué component it is important to state that some did not. Songs such as ‘Riding in the TT races’, ‘Count your blessings and smile’ and ‘It’s in the air’ are cheerful and uplifting family numbers, and he also had a liking for the sentimental ballad, of which ‘Leaning on the lamp-post’ is the best known. That song and several like it contain no salacious content, and if an occasional line slips in it is of a more subtle variety than usual. In the song ‘My little Wigan garden’ Formby describes how his girl will ‘sit on my knee, And watch how the rhubarb grows’[11]. The song ‘I wonder whose under her balcony now’ was due to be included in the 1939 film ‘Trouble Brewing’ until the producers withdrew it due to the following line:
Is he kissing her under the nose,
Or underneath the archway
Where the Sweet William grows. [12]
Many of Formby’s films include a scene in which he sings a sexually suggestive song to an attractive female lead, to her apparent pleasure rather than embarrassment. In the film ‘Much Too Shy’ he actually sings such a song whilst being pedaled along on a bicycle by his younger brother in the film, seemingly a child of 9 or 10 (though actually the diminutive adult actor Jimmy Clitheroe)[13]. Such scenes seem ludicrous or highly inappropriate now, but at the time the Formby persona seemed to render them harmless fun, a private joke with the adults in the audience.
An edition of BBC2’s Late Show in 1990 carried a feature on ‘The cinema of the vulgar’, which included the films of George Formby[14]. The presenter concluded that since the liberalization of attitudes and speech in the 1960s the type of humour embodied by those films, or in Formby’s case the songs they included, has lost much of its’ impact and significance. The music web site I-tunes[15] actually classifies Formby songs as ‘folk music’ and that is perhaps the feeling they evoke when sung or heard today; akin more to sea shanties than pop-tunes; a ‘trip down memory lane’ that still has the power to provoke a schoolboy chuckle.
Bibliography
- Anthony Aldgate & Jeffrey Richards. The British Cinema in the Second World War. Second edition. (Edinburgh: Edinburgh University Press).
- David Brett, George Formby: A Troubled Genius, London: Robson Books, 2001)
- John Fisher, The Entertainers: George Formby, (London: Woburn-Futura, 1975).
- George Formby Complete. Edited by Andrew Bailey and Peter Foss, (London: Wise Publications, 1988).
- John Munday, The British Musical Film. (Manchester University Press, Manchester, 2007).
- George Orwell, The art of Donald McGill, 1943. Reproduced in ‘Essays’, John Carey Ed, pp. 373-384. (London: Everyman Library, 2002).
Other media
- George Formby, The Best of George Formby, Delta Music Ltd, 1996, Track 3 ((music CD).
- Much Too Shy, in Comic Icons: George Formby Collection, , Optimum Classic/Studio Canal, 2007 (DVD collection).
- Cinema of the vulgar. The Late Show, BBC2, 27/2/1990.
- www.itunes.com.
Notes
[1] George Orwell, The art of Donald McGill, 1943. Reproduced in ‘Essays’, John Carey Ed, pp. 373-384 (London: Everyman Library, 2002),p 384.
[2] Anthony Aldgate & Jeffrey Richards. The British Cinema in the Second World War. Second edition. ( Edinburgh: Edinburgh University Press), p.80.
[3] George Formby Complete. Edited by Andrew Bailey and Peter Foss, (London:Wise Publications, 1988) p.88.
[4] George Orwell, The art of Donald McGill, 1943. Reproduced in ‘Essays’, John Carey Ed, pp. 373-384 (London: Everyman Library, 2002),p 376.
[5] For example in Much Too Shy, Comic Icons: George Formby Collection, Optimum Classic/Studio Canal, 2007 (DVD collection).
[6] George Formby Complete. Edited by Andrew Bailey and Peter Foss, (London:Wise Publications, 1988) p. 52.
[7] Ibid, p.192.
[8] Ibid, p.115.
[9] This is from the recorded version: George Formby, The Best of George Formby, Delta Music Ltd, 1996, Track 3 (music CD).
[10]George Formby Complete. Edited by Andrew Bailey and Peter Foss, (London:Wise Publications, 1988) p.132.
[11] John Fisher, The Entertainers: George Formby, (London: Woburn-Futura, 1975) p.31.
[12] David Brett, George Formby: A Troubled Genius, London: Robson Books, 2001), p.83.
[13] Much Too Shy, in Comic Icons: George Formby Collection, Optimum Classic/Studio Canal, 2007.
[14] Cinema of the vulgar. The Late Show, BBC2, 27/2/1990.
[15] www.itunes.com.